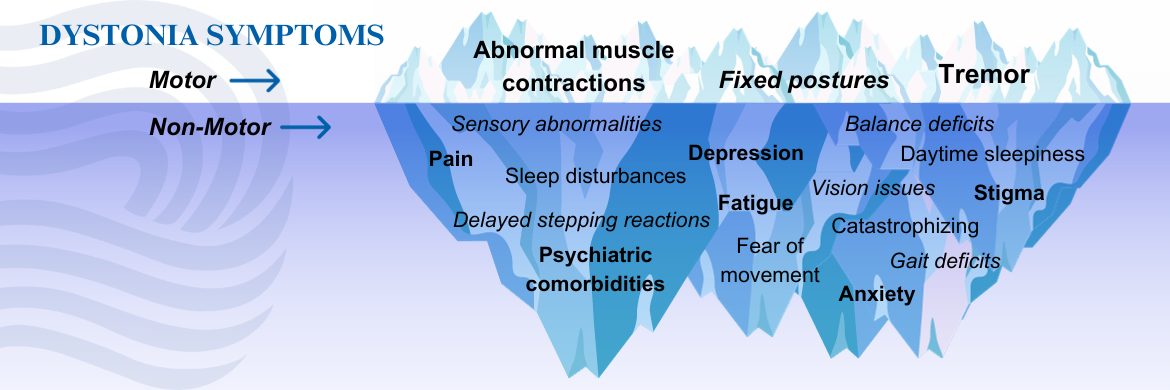
Dystonia is a neurological disorder that affects the physical body, but the impact goes far deeper. Individuals diagnosed with dystonia commonly experience symptoms that affect more than how the body moves. Living well with dystonia often requires addressing more than the physical movement symptoms.
Non-motor symptoms are a significant burden, and can be as disabling—or even more disabling—as the involuntary movements and postures characteristic of dystonia.
If you are experiencing any of the following non-motor symptoms, reach out to your movement disorder specialist for treatment recommendations.
Click here to download a fact sheet on non-motor symptoms of dystonia.
- Mental Health Disorders
Individuals with dystonia are prone to certain mental health disorders, including anxiety and depression. Individuals with dystonia are more likely to experience anxiety and depression than the general population, and at higher rates than individuals with other chronic disorders.
The presence of anxiety and/or depression in individuals with dystonia is among the most reliable predictors of diminished quality of life.
Anxiety
An anxiety disorder differs from simple worry in the following ways:- It is more intense
- It is long-lasting
- It interferes with work, activities, or relationships
Social anxiety disorder is the fear of any situation where public scrutiny may occur, usually with the fear of embarrassment or humiliation. Click here for information about dystonia and social anxiety.
Depression
Clinical depression includes at least one of these two symptoms, nearly every day, for more than two weeks:- An unusually sad mood
- Loss of enjoyment and interest in activities that were once enjoyable
Additional symptoms of clinical depression can include:
- Lack of energy and tiredness
- Feeling worthless or feeling guilty
- Thinking about death or wishing to be dead
- Difficulty concentrating or making decisions
- Moving more slowly, or becoming agitated and unable to settle
- Sleeping difficulties, or sleeping too much
- Loss of interest in food, or eating too much; weight loss or weight gain
- Untreated mental health disorders can have serious and lasting health consequences. If you are experiencing symptoms of depression, anxiety, or additional mental health disorders, ask your movement disorder neurologist or primary care physician for help as a first step toward treatment.
- Sleep Difficulty
Problems with sleep are among the most common and problematic non-motor symptoms associated with dystonia. Sleep disturbances can occur even in cases when the dystonia symptoms are reduced or absent during sleep, and in cases in which the dystonia is well-controlled with treatment.
Click here for more information and recommendations about dystonia and sleep.
- Persistent Pain
Depending on the type of dystonia, pain can be a pervasive and disabling symptom. In many cases, alleviating the dystonic movements and postures will reduce pain. However, alleviating the dystonia symptoms may not alleviate all pain. Depression and sleep disturbance—which are common among dystonia patients—may worsen pain. Dystonia can also cause or worsen painful orthopedic conditions such as arthritis.
- Team Approach to Treating Non-Motor Symptoms
A team of healthcare professionals from multiple disciplines may be necessary to treat the motor and non-motor symptoms associated with dystonia. This can include a movement disorder neurologist, psychiatrist, clinical psychologist, physical therapist, occupational therapist, pain specialist and others depending on your specific needs. Appropriate complementary therapies may provide valuable underlying support to the treatment process and help improve quality of life.
If you are experiencing any of the above symptoms, ask for help from your movement disorder specialist or additional healthcare provider as a first step toward treatment.
- Resources
- BounceBack, a free program by Canadian Mental Health Association (CMHA) for people with mild, low level anxiety or depression
- Mental Health Resources
- Resources for Self-Care in Stressful Times
- Emotional Wellness Toolkit
- My Dystonia & I - A Patient-to-Patient Guide by Merz Therapeutics
- Resources courtesy of Mood Disorders Society of Canada
- Dystonia Wellness Checklist
- Dystonia Information Sessions
- Patient Stories
- More Than Twisting: An In-Depth Look at the Non-Motor Symptoms of Dystonia with Dr. Davide Martino
- From Awareness to Empowerment: Navigating Mental Health with a Neurological Condition presented by Registered Psychotherapist Kristen Drozda
