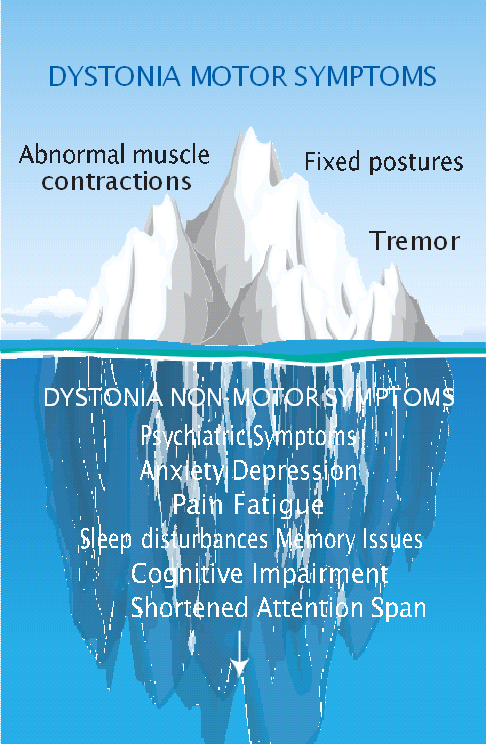
Lurking beneath the surface of dystonia are unseen struggles—the non-motor symptoms that can profoundly impact the lives of those affected. These hidden dimensions, including anxiety, depression, sleep disruption, chronic pain, fatigue, and cognitive impairment, can significantly diminish quality of life.
Understanding the non-motor symptoms of dystonia is crucial for improving the quality of life for dystonia patients. These symptoms significantly impact daily living but often go unnoticed or undertreated. A lack of awareness among healthcare professionals and standardized assessment methods leaves many struggling to get the help they need. By shedding light on these non-motor symptoms, we can equip clinicians with the knowledge and tools to effectively diagnose and manage them, leading to better overall care for individuals with dystonia.
Non-Motor Symptoms of Dystonia Workshop
The Dystonia Medical Research Foundation hosted a virtual scientific workshop, Non-Motor Symptoms of Dystonia, in March 2023. The program was co-chaired by Kathryn Peall, MD, PhD of Cardiff University in the United Kingdom and Davide Martino, MD, PhD of the University of Calgary in Canada. The meeting brought together experts from across the world to discuss the evidence of non-motor symptoms in dystonia, examine existing assessment and treatment methods, and to collaborate on future progress in the field.
This meeting highlighted the DMRF’s commitment to this important topic and reinforced the scientific community’s dedication to focus research to improve the quality of life for patients. The scientific summary was recently published in Dystonia, the DMRF’s scientific journal.
The workshop participants opened the meeting by discussing the importance of researching non-motor symptoms. Identifying the non-motor symptoms of dystonia allows for the development of more holistic treatment plans that address not just the physical manifestations of dystonia, but also the emotional and psychological toll it takes.
By recognizing the pain, fatigue, and anxiety that often accompany dystonia, healthcare professionals can provide targeted therapies and support systems that go beyond simply managing movement control.
Additionally, investigating non-motor symptoms offers a unique window into the underlying mechanisms of dystonia. These seemingly separate features may hold clues to the complex neurological processes at play, potentially leading to breakthroughs in diagnosis and even treatment. By studying the interplay between motor and non- motor symptoms, researchers hope to unlock a deeper understanding of the disease, paving the way for more effective interventions.
The workshop looked at this issue from several perspectives, breaking down the non-motor symptoms into different categories. Workshop faculty shared the current research in each topic before providing insight into the future of non-motor research.
- Psychiatric Symptoms
Psychiatric symptoms are the most studied non-motor symptoms of dystonia. Most studies examine the prevalence of anxiety and depression in different types of dystonia patients compared to a control group. Indeed, patients with cervical dystonia, blepharospasm, spasmodic dysphonia, focal hand dystonia, writer’s cramp, and musician’s dystonia reported more instances of anxiety and depression than the respective control groups.
Why is this the case? Researchers are still working to find an answer. And while some might assume that mental health concerns follow a dystonia diagnosis, some studies have shown the opposite. Indeed, some research has found that psychiatric symptoms were present in patients before their motor symptoms began. The areas of the brain thought to be related to mental health conditions are also the areas of the brain affected by dystonia, indicating that there may be a link. Further research is needed to further examine this phenomenon.
- Pain
The effect of chronic pain on quality of life is well-documented, both with dystonia patients and others. In fact, cervical dystonia patients report chronic pain more frequently than any other non-motor symptom. Researchers are developing new tools to study pain in dystonia further. This includes the development of new rating scales, which allow patients to better assess and define their experience. The scales provide a consistent way to measure feelings of pain, which will allow researchers to compare patient experiences more broadly. While more work needs to be done in this topic, studies have shown that injectable botulinum toxin can help reduce pain.
- Sleep Disruption and Fatigue
Studies on the effects of sleep disruption on dystonia patients are very limited. Sleep is critical to a healthy brain—a good night of uninterrupted sleep allows the brain to slow its activity, to reset and repair itself, and to adapt to meet any anticipated needs. Research on the motor symptoms of dystonia has found that brain plasticity, or the ability of the brain to rewire itself in response to certain internal and external influences, is intrinsically connected to the disease itself. Researchers believe therefore that the inability to get a good night’s rest might exacerbate these symptoms.
Fatigue, or the perception of physical and mental effort, is also understudied in dystonia. Researchers are working to develop sleep studies to better measure the effects of sleep and fatigue on the disorder.
- Cognitive Dysfunction
Executive function, defined as a set of mental skills that include working memory, flexible thinking, and self- control, is the only form of cognitive ability to be consistently studied and disrupted by dystonia. Studies have found patients struggle with sustained attention, complex movement planning and visuospatial working memory, which refers to the ability to recall shapes and colors along with their location and movements. For some DBS patients, cognitive function improves after surgery. For other dystonia patients, more research is needed to best understand this symptom.
- Pediatric Dystonia
Little research has been conducted on non-motor symptoms in children with dystonia. Participants in the workshop discussed whether children and young adults should be treated and studied separately than adults, or if using the same tools to study patients from childhood through adulthood would more accurately capture symptoms. In either case, researchers are developing measurements best suited for this patient population.
- Models of Care
The meeting ended with a discussion about improving models of care to comprehensively address motor and non-motor symptoms of dystonia.
Many dystonia patients visit their doctor on a quarterly basis for brief appointments centered around botulinum toxin injections. The appointments rarely involve the screening, assessment, or management of non-motor symptoms, much to the dissatisfaction of patients. Instead, management of these symptoms often becomes the responsibility of primary care doctors who lack the specialized knowledge on how these symptoms connect. If movement disorder specialists aren’t trained to recognize the significance of non-motor symptoms, they may be missing key indicators of the disease. Additionally, patients may begin to think that their non-motor symptoms are less important than their motor symptoms and fail to report them, creating a cycle that may be difficult to counteract.
Screening for non-motor symptoms in dystonia could be an important first step in better treatment options and more quantitative data to assist further studies. Many other movement disorders have screeners to this end, and the researchers involved in the workshop are interested in developing a similar screener for dystonia patients.
In conclusion, research into the non-motor symptoms of dystonia is not just about alleviating discomfort; it’s about unlocking a deeper understanding of the brain and its complexities. By delving into these hidden dimensions, we pave the way for more effective treatments, potentially even prevention for a wider range of neurological conditions. The DMRF’s unwavering dedication to this critical research, coupled with their unwavering support, for the dystonia community, is a beacon of hope in the ongoing quest to conquer this challenging disorder.
Those interested in reading the complete article in the journal Dystonia can find it here.
You can request or download a fact sheet on this topic here.
Reprinted and adapted with permission from DMRF Dystonia Dialogue, Spring 2024 Vol 47, No 1.
